In Summary
- Over 220,000 cholera cases have been reported in Africa in early 2025, yet case-fatality rates are lower than in previous years in many high-burden nations.
- Major vaccination campaigns reached millions in early 2025 despite a global shortage of oral cholera vaccines.
- Floods, conflict, and urban growth remain key drivers, but coordinated efforts by African nations are steadily improving response capacity.
Deep Dive!!
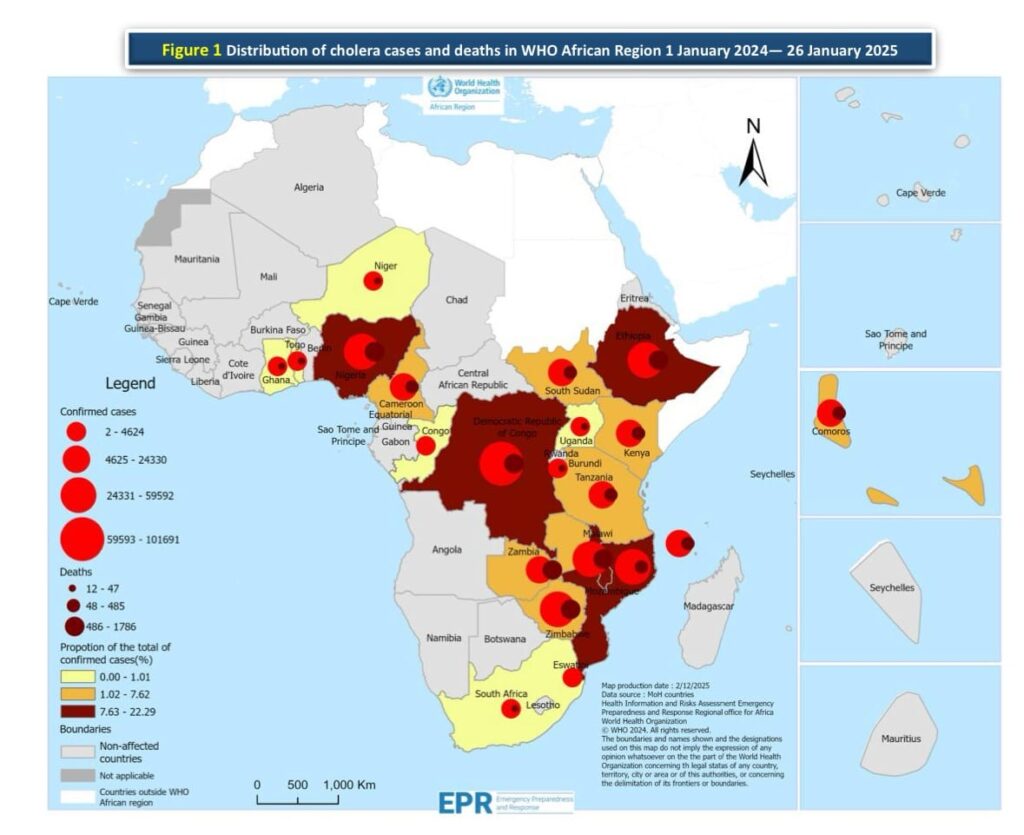
Lagos, Nigeria Saturday, August 23 – Cholera remains one of the most persistent health threats in Africa, with 2025 continuing a trend of outbreaks linked to contaminated water sources, and climate-related events. By mid-2025, the World Health Organization reported over 220,000 suspected cases across 16 African countries, with the highest concentrations in eastern and central regions.
Still, the situation is not defined by numbers alone. Case fatality rates have dropped in several high-burden countries compared to 2024, largely due to faster detection, community-based treatment, and mass oral cholera vaccine (OCV) campaigns. Over 10 million vaccine doses have been administered across Africa this year, even as global supplies remain limited. Investments in water infrastructure, new boreholes, emergency chlorination points, and repairs to flood-damaged pipelines are changing the trajectory in some areas.
In this must read article, we bring you the ten African countries most affected by cholera in 2025, based on verified case data and reported outbreaks. Each profile explores the scale of the crisis, the main factors driving transmission, and the actions being taken on the ground. Together, they provide a clear picture of where Africa stands in its relentless and seemingly succeeding fight against cholera today.
10. Togo
Togo reported 88 suspected cholera cases and 2 deaths in early 2025, giving it a case fatality rate of 2.3%. The cases were concentrated in the Maritime and Plateaux regions, with outbreaks emerging after heavy rains contaminated local water sources. Limited access to safe drinking water in rural communities has historically made these areas vulnerable to waterborne diseases, and this year’s floods disrupted already fragile sanitation systems.
In response, Togo’s Ministry of Health, with support from UNICEF and WHO, has deployed mobile teams to chlorinate wells and train local health workers in early detection. Oral rehydration corners have been set up in health posts across affected districts, reducing the delay in treatment and helping to keep fatalities low despite limited resources. Plans for an oral cholera vaccine campaign targeting high-risk villages are underway, with doses expected by the last quarter of 2025.
9. Zimbabwe
Zimbabwe recorded 92 suspected cholera cases and 2 deaths in 2025, resulting in a case fatality rate of 2.2%. The majority of these cases were reported in Manicaland and Harare provinces, areas that have historically struggled with waterborne diseases due to aging water infrastructure and periodic urban water shortages.
The Ministry of Health and Child Care, in collaboration with Médecins Sans Frontières and the Africa CDC, has reactivated cholera treatment units in high-risk districts and improved community-based surveillance. Door-to-door health education campaigns, combined with the distribution of water purification tablets, have been critical in reducing household transmission. Although Zimbabwe did not receive oral cholera vaccines in early 2025 due to global stockpile shortages, preparations are in place for a targeted campaign once supplies improve.
8. Uganda
Uganda reported 108 suspected cholera cases and 1 death in early 2025, giving a case fatality rate of 0.9%. Most of these cases were detected in refugee-hosting districts in the West Nile sub-region, particularly around Yumbe and Obongi, where large settlements rely on communal water sources. These areas have long been vulnerable to cholera due to overcrowding and challenges in maintaining sanitation during seasonal rains.
The 2025 cases emerged after heavy rainfall in March caused flooding that contaminated shallow wells and open water sources. Uganda’s Ministry of Health, supported by the United Nations High Commissioner for Refugees (UNHCR) and UNICEF, responded by intensifying water chlorination, repairing boreholes, and increasing health promotion activities in settlements. Rapid response teams were deployed within 48 hours of the first alerts, limiting the outbreak’s spread.
Uganda’s national preparedness plan, developed in 2023, has proven effective in reducing cholera’s impact. The presence of pre-trained village health teams meant that cases were quickly identified and treated, preventing a wider epidemic. The country is also in line to receive oral cholera vaccines for refugee-hosting districts later in 2025, a move expected to strengthen future prevention efforts.
7. Ethiopia
Ethiopia has reported 129 suspected cholera cases and 1 death in 2025, with a case fatality rate of 0.8%. Most cases have been concentrated in the Somali and Oromia regions, areas prone to cholera outbreaks due to recurrent droughts, displacement, and limited access to clean water. In early 2025, flash floods following heavy rains contaminated water points in parts of the Somali region, triggering localized transmission.
The Ministry of Health, working with the Africa CDC and World Health Organization, has implemented a multi-pronged response. Emergency water trucking and chlorination campaigns were launched within days of the first reported cases. Health workers trained under Ethiopia’s 2024 National Cholera Preparedness Plan have been active in case management and surveillance, ensuring patients receive oral rehydration and intravenous fluids promptly.
Ethiopia’s efforts to integrate cholera prevention into broader health and humanitarian responses have shown results. Despite challenging conditions, early detection and rapid treatment have kept the case fatality rate below 1%. Plans for a mass oral cholera vaccination campaign in high-risk districts are scheduled for late 2025, alongside ongoing investments in borehole rehabilitation to strengthen long-term water access.
6. Nigeria
Nigeria recorded 835 suspected cholera cases in 2025 with a case fatality rate of 2.0%. Outbreaks were reported mainly in the northeastern states of Borno, Yobe, and Adamawa, regions affected by prolonged conflict and displacement. Overcrowded camps for internally displaced persons (IDPs), coupled with inadequate sanitation facilities, created conditions for the disease to spread during seasonal rains.
The Nigeria Centre for Disease Control and Prevention (NCDC) has led the response, activating rapid response teams in all affected states. Supported by the World Health Organization and UNICEF, the government expanded access to safe drinking water through borehole rehabilitation, chlorination of public water points, and distribution of water purification tablets. Cholera treatment centers were set up in Maiduguri and other high-burden areas, ensuring timely care and reducing fatality rates compared to previous years.
Despite a global shortage of oral cholera vaccines, Nigeria successfully secured doses for a targeted campaign in high-risk LGAs, set to begin in late 2025. This comes alongside community health education drives promoting handwashing and safe water storage, led by local volunteers and health workers.
5. Ghana
Ghana has reported 948 suspected cholera cases and 7 deaths in 2025, resulting in a case fatality rate of 0.7%. The bulk of these cases emerged in the coastal regions, particularly Greater Accra and the Central Region, where rapid urbanization has outpaced sanitation infrastructure. Heavy rains in June 2025 caused flooding in low-lying neighborhoods, contaminating water sources and overwhelming drainage systems.
The Ghana Health Service responded by activating its National Public Health Emergency Operations Centre to coordinate the outbreak response. With support from the World Health Organization and local NGOs, authorities have distributed oral rehydration salts to health facilities, deployed mobile rapid response teams to affected communities, and initiated household-level disinfection campaigns. Public awareness drives through radio and community gatherings have played a key role in early treatment-seeking, contributing to the country’s low fatality rate.
Ghana’s preparedness has been strengthened by its adoption of a national cholera control plan in 2024, which emphasized pre-positioning medical supplies and training district health officers. Plans are underway to introduce oral cholera vaccines in high-risk coastal districts by the end of 2025, marking a significant step toward long-term prevention.
4. Angola
Angola recorded 1,153 suspected cholera cases and 48 deaths in 2025, resulting in a case fatality rate of 4.2%. Most cases have been concentrated in the provinces of Luanda and Benguela, where dense urban settlements face ongoing challenges with waste management and access to clean water. The outbreak intensified in March 2025 after heavy rains caused flooding in informal settlements, leading to widespread contamination of shallow wells and open drainage systems.
The Ministry of Health, working with the Africa CDC and UNICEF, has launched emergency measures including the rehabilitation of key water supply systems in Luanda, mass chlorination of water sources, and the deployment of rapid response teams. Cholera treatment centers have been re-established in high-burden districts, supported by international NGOs, to ensure immediate case management. Despite these efforts, limited diagnostic capacity and delayed reporting in some areas have hindered early containment.
In response to rising fatalities, Angola has prioritized the procurement of oral cholera vaccines through the global stockpile and plans to begin a nationwide vaccination campaign in the second half of 2025, focusing on densely populated urban neighborhoods. The government has also announced a new urban sanitation initiative aimed at reducing long-term vulnerability to waterborne diseases.
3. Tanzania
Tanzania has reported 1,434 suspected cholera cases and 7 deaths in 2025, giving a case fatality rate of 0.5%. Outbreaks have been concentrated in coastal and lake-bordering regions, particularly around Dar es Salaam and areas along Lake Victoria. Seasonal rains in early 2025 caused localized flooding, contaminating water sources and accelerating transmission in fishing communities and informal urban settlements.
The Ministry of Health has coordinated a nationwide response through its National Cholera Task Force, activating rapid response teams and improving surveillance at district levels. Supported by the World Health Organization and the Global Task Force on Cholera Control (GTFCC), Tanzania conducted targeted oral cholera vaccination campaigns in Mwanza and Pwani regions, reaching over 600,000 people by May 2025. These campaigns, combined with extensive public health education efforts, have kept fatalities among the lowest in the region. Infrastructure improvements have also been a focus. New boreholes have been drilled in high-risk rural districts, and emergency repairs were made to damaged water pipelines in Dar es Salaam.
2. Democratic Republic of Congo (DRC)
The Democratic Republic of Congo has recorded 4,007 suspected cholera cases and 75 deaths in 2025, resulting in a case fatality rate of 1.9%. The majority of these cases have been reported in the eastern provinces of North Kivu, South Kivu, and Ituri which are affected by conflict, population displacement, and limited access to safe water. Camps for internally displaced persons, often overcrowded and lacking proper sanitation, have been the epicenters of transmission.
The Ministry of Health, supported by the Africa CDC, WHO, and Médecins Sans Frontières, has deployed rapid response teams to outbreak hotspots and reopened cholera treatment centers in North Kivu. Over 1 million liters of water have been trucked to affected camps since March, while local health workers have been trained to manage cases at the community level, reducing delays in treatment.
Despite the challenges of insecurity, the DRC has made progress in expanding access to preventive measures. The government, with international partners, secured doses for an oral cholera vaccine campaign targeting 500,000 people in high-risk zones. Additionally, surveillance systems have been strengthened with mobile reporting tools that allow real-time tracking of new cases, a critical step toward faster containment.
1. South Sudan
South Sudan has reported 11,116 suspected cholera cases and 174 deaths in 2025, giving it a case fatality rate of 1.6%. The outbreak has been most severe in the states of Jonglei, Upper Nile, and Unity, where extensive flooding in early 2025 displaced thousands of people and contaminated major water sources. Overcrowded displacement camps, inadequate sanitation, and limited access to medical care have fueled transmission.
The Ministry of Health, supported by WHO, UNICEF, and the Africa CDC, has launched one of the largest cholera response operations on the continent. Over 20 cholera treatment centers have been established in high-burden counties, and more than 3 million liters of safe water are being supplied weekly to affected communities. A mass oral cholera vaccination campaign reached over 900,000 people by June 2025, significantly reducing new infections in targeted areas. Also, ongoing investments in early-warning surveillance systems and expanded community health networks are improving the country’s ability to detect and treat cases quickly.
https://www.africanexponent.com/top-10-african-countries-with-the-highest-rates-of-cholera-as-of-early-2025/