On some degree, the human liver within the working room at Northwestern Memorial Hospital in Chicago was alive. Blood circulating by means of its tissues delivered oxygen and eliminated waste merchandise, and the organ produced bile and proteins which are important to the physique.
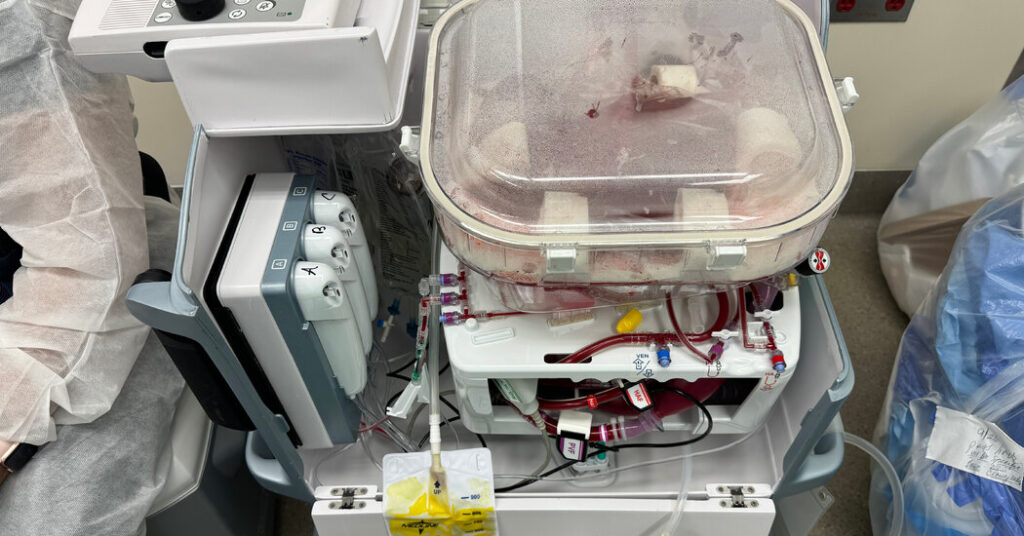
But the donor had died a day earlier, and the liver lay inside a boxy plastic machine. The organ owed its vitality to this machine, which was preserving it for transplantation right into a needy affected person.
“It’s a little bit science fiction,” mentioned Dr. Daniel Borja-Cacho, a transplant surgeon on the hospital.
Surgeons are experimenting with organs from genetically modified animals, hinting at a future once they might be a supply for transplants. But the sector is already present process a paradigm shift, pushed by applied sciences in widespread use that permit clinicians to briefly retailer organs exterior the physique.
Perfusion, as its known as, is altering each side of the organ transplant course of, from the way in which surgeons function, to the varieties of sufferers who can donate organs, to the outcomes for recipients.
Most considerably, surgical applications which have adopted perfusion are transplanting extra organs.
Since 2020, Northwestern has had a 30 p.c uptick in its quantity of liver transplants. Nationally, the variety of lung, liver and coronary heart transplants every rose by greater than 10 p.c in 2023, one of many largest year-over-year will increase in a long time.
Without blood circulate, organs quickly deteriorate. That’s why clinicians have lengthy thought of the perfect organ donor to be somebody who died underneath circumstances that ended mind exercise however whose coronary heart continued beating, holding the organs viable till they might be matched with recipients.
To reduce damage to organs after their removing from a donor’s blood provide and earlier than they’re linked to a recipient’s, surgeons used to chill them to simply above freezing, considerably slowing their metabolic processes.
This extends the window during which organs will be transplanted, however solely briefly. Livers stay viable for not than 12 hours, and lungs and hearts nearer to 6.
Scientists have lengthy experimented with methods for holding organs in additional dynamic circumstances, at a hotter temperature and perfused with blood or one other oxygenated resolution. After years of growth, the primary machine for preserving lungs through perfusion received approval from the Food and Drug Administration in 2019. Devices for perfusing hearts and livers have been accredited in late 2021.
The units primarily pump blood or an oxygenated fluid by means of tubes into the blood vessels of the donated organ. Because cells in a perfused organ proceed to operate, clinicians can higher assess whether or not the organ will thrive in a recipient’s physique.
Bolstered by that info, transplant surgeons have begun to make use of organs from older or sicker donors that they may in any other case have turned down, mentioned Dr. Kris Croome, a professor of surgical procedure on the Mayo Clinic in Florida. “We’re going after organs we never would have before, and we’re seeing good outcomes,” he mentioned.
Perfusion additionally eases the grueling means of organ restoration and transplant, hourslong surgical procedures that medical doctors usually conduct towards the clock, starting in the course of the evening and accomplished in back-to-back succession.
Now surgical groups can get well an organ, perfuse it in a single day whereas they sleep and full the transplant within the morning with out worry that the delay may have broken the organ.
Perhaps most vital, perfusion has additional opened the door to organ donation by comatose sufferers whose households have withdrawn life help, permitting their hearts to ultimately cease. Each yr, tens of hundreds of individuals die this fashion, after the cessation of circulation, however they have been not often donor candidates as a result of the dying course of disadvantaged their organs of oxygen.
Now, surgeons are perfusing these organs, both by eradicating them to a machine or, in a lower-tech method, by recirculating blood in that area of the donor’s physique. And that has made them way more interesting for transplant.
Since 2020, the variety of livers transplanted after the circulatory demise of the donor has doubled, in line with an evaluation of information from the United Network for Organ Sharing, the nonprofit that runs the United States’ transplant system.
Once, surgeons by no means used hearts from such donors due to that organ’s sensitivity to oxygen deprivation; in 2023, due to perfusion, they transplanted over 600.
By tapping this new cadre of donors, transplant facilities mentioned they may discover organs extra shortly for the surplus of sufferers in pressing want. Dr. Shimul Shah mentioned the organ transplant program he directs on the University of Cincinnati had primarily worn out its ready record for livers. “I never thought, in my career, I would ever say that,” he mentioned.
One impediment to the adoption of the expertise could also be price. At the charges presently demanded by machine makers, perfusing an organ exterior the physique can add greater than $65,000 to the value of a transplant; smaller hospitals could not be capable of justify the upfront expense.
One of the main firms, TransMedics, raised its costs considerably after regulators accredited its machine, prompting a stern letter from Representative Paul Gosar, Republican of Arizona, who wrote: “What began as a promising medical equipment innovation and an opportunity to increase transplantation nationwide is now being held hostage by a public company that has lost its true north.”
But some surgeons mentioned that the expertise would possibly nonetheless lower your expenses, since sufferers who obtain perfused organs typically go away the hospital faster and with fewer problems, and have higher medium- and long-term outcomes.
Surgeons are nonetheless exploring the higher limits of how lengthy perfused organs can survive exterior the physique, and as considerably because the applied sciences are already altering transplant, some say that is solely the start.
Dr. Shaf Keshavjee, a surgeon on the University of Toronto whose lab was on the forefront of growing applied sciences to protect lungs exterior the physique, mentioned the units might ultimately permit medical doctors to take away, restore and return lungs to sick sufferers moderately than substitute them. “I think we can make organs that will outlive the recipient you put them in,” he mentioned.
Dr. Ashish Shah, the chairman of cardiac surgical procedure at Vanderbilt University, one of many busiest coronary heart transplant applications within the nation, agreed, calling that “the holy grail.”
“Your heart sucks,” he mentioned. “I take it out. I put it on my apparatus. While you don’t have a heart, I can support you with an artificial heart for a little while. I then take your heart and fix it — cells, mitochondria, gene therapy, whatever — and then I sew it back in. Your own heart. That’s what we’re really working for.”