A committee of independent advisers to the Food and Drug Administration voted unanimously on Monday that the benefits outweigh the risks of the newest experimental drug for Alzheimer’s disease.
Alzheimer’s afflicts more than six million Americans. It has no cure, and there is no treatment or lifestyle modification that can restore memory loss or reverse cognitive decline.
The drug, made by Eli Lilly, is donanemab. It modestly slowed cognitive decline in patients in the early stages of the disease but also had significant safety risks, including swelling and bleeding in the brain.
The committee concluded, though, that the consequences of Alzheimer’s are so dire that even a modest benefit can be worthwhile.
The F.D.A. usually follows the advice of the agency’s advisory committees but not always.
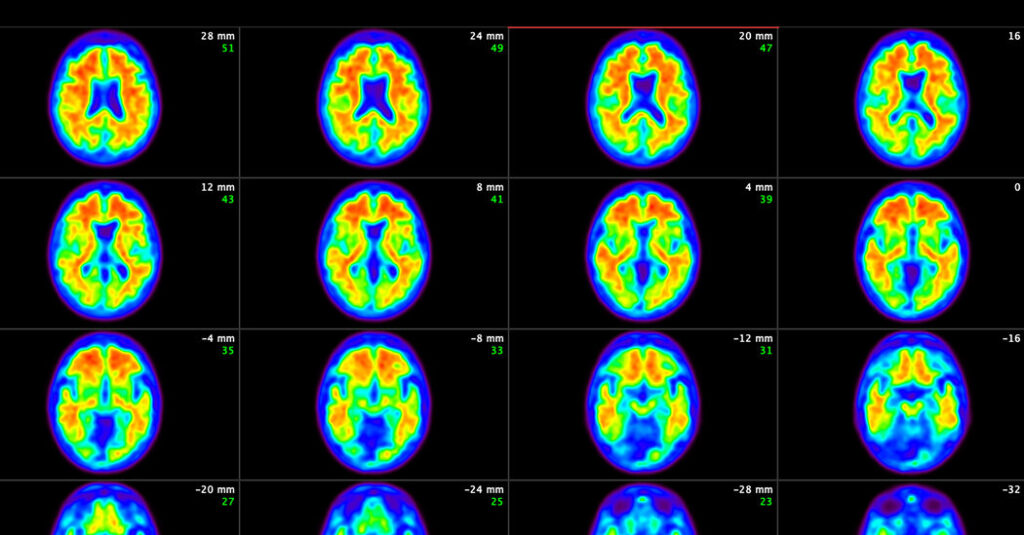
The drug is based on a long-held hypothesis that Alzheimer’s disease begins when rough hard balls of amyloid, a protein, pile up in patients’ brains, followed by a cascade of reactions leading to the death of neurons.
The idea is to treat Alzheimer’s by attacking amyloid, clearing it from the brain. Two similar amyloid-fighting drugs were approved recently: Leqembi, made by Eisai and Biogen, was approved last year. That drug’s risks and modest benefits are similar to those of donanemab. Aduhelm, made by Biogen, is the other drug and was approved in 2021 but was discontinued because there was insufficient evidence that it could benefit patients.
Donanemab was expected to be approved earlier this year, but in March, the F.D.A. decided that, instead, it would require donanemab to undergo the scrutiny of an independent advisory committee, a surprise to Eli Lilly.
The vote, said Dr. Daniel Skovronsky, chief medical and scientific officer at Lilly, confirmed his 25-year quest to find a way to intervene in the Alzheimer’s disease. Now, he said, the company is starting a study that, it hopes, will stop the disease before symptoms even begin.
At issue before the committee on Monday were some unusual aspects of donanemab’s clinical trials, especially that study participants stopped taking the drug as soon as their amyloid was cleared. Some experts questioned whether stopping was the best strategy and whether clinical practice should include halting the treatment after amyloid clearance.
Donanemab, like Leqembi, is given as intravenous infusions. Alzheimer’s experts said that the drugs’ effects in slowing cognitive decline are so modest that they might not be noticeable to patients and families. Also, some noted, patients and families would have no way of knowing how the disease would have progressed without the treatment.
Lilly submitted data from a 76-week study of 1,736 people in the early stages of the disease, with either mild cognitive impairment or mild dementia. The participants were randomly assigned to get donanemab or a placebo. To measure effectiveness, the Lilly researchers assessed the patients’ performance on cognitive tests.
Cognitive decline slowed by about 4½ to 7½ months in those taking donanemab compared with those who got the placebo. Nearly half who took donanemab stayed at the same cognitive level one year into the study, compared with 29 percent who got the placebo.
But, the committee noted, nearly all study participants were white.
“I would like to see more data on underrepresented groups,” Colette C. Johnson, a patient representative on the committee, said.
Three patients taking donanemab died with brain swelling or bleeding that was linked to the drug. The F.D.A. wanted a more detailed analysis of the deaths of trial participants to check for other serious safety problems. Lilly complied and reported that no evidence suggested additional deaths were caused by the drug.
Lilly’s decision to stop treating patients as soon as a brain scan indicated donanemab had cleared their amyloid had real appeal, committee members said. Patients could avoid monthly infusions and some of the risks of treatment. And costs might be lower.
In a briefing document, Lilly suggested that continuing the drug after amyloid is gone would not help patients and might be harmful. “Once the target is cleared from the brain, continued dosing of donanemab is likely not beneficial and only adds to treatment burden and potential risks,” the company wrote.
The committee liked the aspect of halting treatment but had questions.
Sarah Dolan, a panel member representing consumers, said that the possibility of stopping treatment “could actually be a motivational factor for patients to stay compliant.” But, she said, “there will always be a concern in the back of their head: Is it coming back? Am I getting worse?”
Dr. Constantino Iadecola of Weill Cornell Medicine noted that it was not clear how to monitor patients after they stop taking the drug. “Monitoring is going to be necessary,” he said. And, he added, “how soon will you have to intervene if you have a signal of amyloid going up?”
Lilly scientists have estimated it would take nearly four years for amyloid levels to bump up over the threshold again.
Another unusual feature involved the company’s decision to scan patients’ brains for tau, a tangled spaghetti-like protein that appears in brains after amyloid accumulates. The more tau, the worse the cognitive decline.
Trial participants with intermediate tau levels — indicating an earlier stage of the disease — declined more slowly on donanemab than those whose levels were high — supporting a widespread theory that treating patients as early as possible provides a better chance of slowing symptoms.
That raised a question of whether patients should have tau brain scans before starting the drug.
In its briefing document, Lilly said it was not recommending that tau scanning be required. “The measurement of tau levels is not standardized and therefore could not be readily implemented in routine clinical practice,” the company said. The F.D.A., in its review, said that based on the evidence so far, there did not seem to be a reason for patients to be tested for tau before receiving donanemab.
Committee members had the same reaction.
“From a practical perspective I think this would not be a wise thing to have as a barrier,” Dr. Kathleen L. Poston, a neurology professor at Stanford, said.
In the end, these drugs may be just a foothold in the search for an effective treatment. But, as the committee heard, for patients and their families, the possibility of slowing the progress of Alzheimer’s, even by a few months, can be tantalizing.
“There is a huge unmet need here,” said Ms. Dolan, the panel’s consumer representative.